Connect With Us
Blog

Reasons for Pins and Needles in the Feet

Pins and needles in the feet, medically known as paresthesia, can arise from a variety of causes that often involve the nerves in the feet, toes, or ankles. Diabetes and alcohol abuse frequently lead to peripheral neuropathy, where prolonged high blood sugar levels damage the nerves, resulting in tingling or numbness. Tarsal tunnel syndrome, caused by compression of the tibial nerve in the ankle, is another possible cause of burning and tingling pain. Vitamin deficiencies, particularly B12, may also contribute to nerve dysfunction, resulting in tingling sensations. Inherited conditions like Charcot-Marie-Tooth disease can weaken the peripheral nerves and cause persistent tingling and numbness. Exposure to certain toxins or medications can similarly affect nerve health. A podiatrist can evaluate your symptoms through a physical exam, diagnostic tests, and a review of your medical history to determine the underlying cause. If you frequently experience a feeling of pins and needles in your feet, it is suggested that you schedule an appointment with a podiatrist for a thorough exam.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
See Your Foot Specialist Regularly If You Work On Your Feet
Understanding Plantar Fasciitis
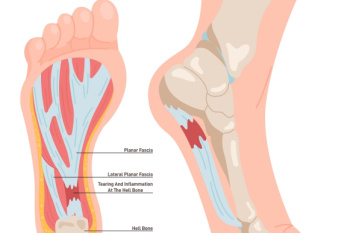
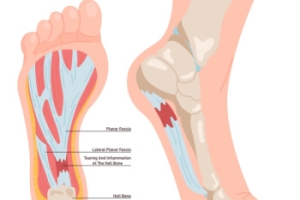
Plantar fasciitis is a common condition that causes pain in the heel and bottom of the foot. The primary cause of plantar fasciitis is repeated stress or strain on the fascia, often due to excessive walking, running, or standing. Other factors like wearing poor footwear, tight calf muscles, or being overweight can also contribute. The most noticeable symptom is sharp pain in the heel, especially when taking the first steps in the morning or after periods of rest. As the day progresses, the pain may lessen but can return with prolonged standing or walking. Diagnosis typically involves a physical examination where a podiatrist may palpate the heel and foot, and sometimes imaging tests to rule out other conditions. If you have heel pain, it is suggested that you contact a podiatrist who can accurately diagnose and treat plantar fasciitis.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Tibialis Posterior Rupture

A tibialis posterior rupture is a significant injury involving the tendon that supports the arch of the foot and aids in stability during walking. This tendon is essential for proper foot movement and alignment. Ruptures are often caused by overuse, trauma, or degenerative changes, particularly in individuals with flat feet or those involved in repetitive, high-impact activities. Symptoms include pain along the inner ankle or foot, swelling, difficulty walking, and progressive flattening of the arch. Left untreated, the condition can lead to severe flatfoot deformity and impaired mobility. Diagnosis typically involves a clinical exam, imaging like an MRI scan, and functional assessments. Treatment options range from rest, bracing, and targeted exercises, to surgical repair for severe cases. Early intervention is essential for optimal recovery. If you suspect such a rupture, it is suggested that you consult a podiatrist for evaluation and a tailored treatment plan.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendonitis
- Achilles tendon rupture
- Stress fractures
- Bursitis
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Various Causes of Ankle Pain
Ankles are joints that connect bones in the feet with bones in the lower leg. They are comprised of bones, ligaments, muscles, tendons, blood vessels, and nerves. The ankle joint allows the foot to move side-to-side, as well as up-and-down.
Ankle pain can be caused by a variety of conditions, but is most commonly due to soft tissue injuries such as ankle sprains and strains.
An ankle sprain occurs when one or more of the strong ligaments that support and stabilize the ankle become overly stretched or even torn if the ankle rolls, turns, or twists awkwardly. Depending on the grade of sprain (mild-moderate-severe), there will be varying degrees of pain, swelling, and restricted range of motion, along with tenderness, bruising, and ankle instability. There may even be an audible popping noise at the moment of injury.
Ankle strains can sometimes produce similar symptoms of pain, swelling, and loss of motion, however, they are due to overly stretched muscles and tendons—not ligaments. Ankle strains may also cause muscle cramps in the feet, calves and shins.
Ankle fractures are another common source of ankle pain and occur one or more of the three bones in the ankle become fractured (broken). These breaks can be stress fractures (due to repetitive stress) or traumatic fractures (due to an acute injury). Depending on where and how severe the fracture is, symptoms can include pain and swelling that can sometimes spread up to the knee, bruising or discoloration, and an inability to bear weight. A visible deformity or exposed bone may occur in severe fractures.
Various forms of arthritis may also cause ankle pain. Rheumatoid arthritis (RA) causes the immune system to attack healthy joints, like the ankle joint, by mistake, causing stiffness and swelling in both ankles. Osteoarthritis occurs when cartilage covering the ends of bones wears down, causing the bones to rub against each other. This results in pain, stiffness, and reduced range of motion in the ankle. Gout is a form of arthritis where excess amounts of uric acid in the bloodstream crystallize and build up on joints, causing severe pain and swelling. Reactive arthritis causes joint pain and swelling in the ankle in response to an infection in another part of the body.
Other forms of ankle pain include bursitis (an inflammation of a cushioning bursa sac between tendons and bone), scleroderma (a thickening of connective tissues), chronic ankle instability (caused by improperly healed ankle sprains), Achilles tendon injuries, flat feet, or an infection in the ankle.
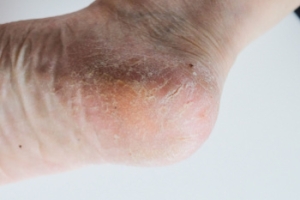
Causes of Cracked Heels
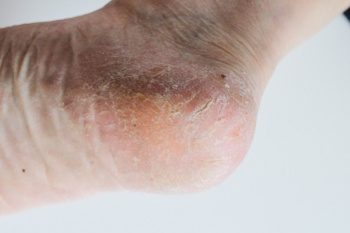
Cracked heels, also known as heel fissures, can be caused by various factors that affect foot health. Diabetes can lead to poor circulation and dry skin, increasing the risk of cracked heels. Hypothyroidism, a condition where the thyroid does not produce enough hormones, can also cause dry skin and thickened skin around the heels. Skin conditions like psoriasis and eczema can contribute to cracked heels due to dryness and irritation. Fungal infections, such as athlete’s foot, can cause the skin on the feet to peel, crack, and become inflamed. Additionally, a vitamin deficiency, especially in zinc or omega-3 fatty acids, can lead to skin issues, including cracked heels. Keeping feet moisturized, treating underlying health conditions, and practicing proper foot care are essential to prevent and manage cracked heels. Cracked heels can be painful and unsightly. If you have developed this condition, it is suggested that you schedule an appointment with a podiatrist who can successfully treat cracked heels, which often includes prescribed medication.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Ankle Sprains in Athletes

Ankle sprains are one of the most common injuries in athletes, caused by overstretching or tearing the ligaments that stabilize the joint. They often occur during sudden movements like jumping, pivoting, or uneven landings. Each sprain is unique, ranging from mild to severe, depending on the extent of ligament damage. Symptoms include pain, swelling, bruising, and difficulty bearing weight. Immediate care involves rest, which helps reduce swelling and pain. However, more severe sprains may require medical attention and targeted stretching to ensure proper healing and avoid long-term instability. Prevention strategies include strengthening exercises, ankle taping, wearing supportive footwear, and avoiding risky movements. If you have persistent pain or repeated ankle sprains, it is suggested that you schedule an appointment with a podiatrist to develop a treatment plan and ensure a safe return to sports.
Ankle and foot injuries are common among athletes and in many sports. They can be caused by several problems and may be potentially serious. If you are feeling pain or think you were injured in a sporting event or when exercising, consult with Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries
The most common injuries that occur in sporting activities include:
- Achilles Tendonitis
- Achilles Tendon Rupture
- Ankle Sprains
- Broken Foot
- Plantar Fasciitis
- Stress Fractures
- Turf Toe
Symptoms
Symptoms vary depending upon the injury and in some cases, there may be no symptoms at all. However, in most cases, some form of symptom is experienced. Pain, aching, burning, bruising, tenderness, tightness or stiffness, sensation loss, difficulty moving, and swelling are the most common symptoms.
Treatment
Just as symptoms vary depending upon the injury, so do treatment options. A common treatment method is known as the RICE method. This method involves rest, applying ice, compression and elevating the afflicted foot or ankle. If the injury appears to be more serious, surgery might be required, such as arthroscopic or reconstructive surgery. Lastly, rehabilitation or therapy might be needed to gain full functionality in the afflicted area. Any discomfort experienced by an athlete must be evaluated by a licensed, reputable medical professional.
If you have any questions, please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.