Connect With Us
Blog
Items filtered by date: December 2021
How Gout Differs From Rheumatoid Arthritis

Gout and rheumatoid arthritis, also known as RA, are two distinct medical conditions that can affect joints in the feet and ankles, and they can be differentiated based on various factors. Gout is caused by the accumulation of uric acid crystals in the joints, usually due to an overproduction or under-excretion of uric acid. In contrast, RA is an autoimmune disease where the body's immune system mistakenly attacks its own joints, leading to inflammation. The symptoms of gout and RA also vary. Gout typically presents with sudden and intense pain in one joint, often the big toe, along with redness and swelling. RA, on the other hand, typically affects multiple joints symmetrically and causes chronic pain, morning stiffness, and joint deformities over time. Laboratory tests can help distinguish between the two conditions. Elevated levels of uric acid in the blood or the presence of uric acid crystals in joint fluid are indicative of gout. RA is characterized by the presence of specific auto-antibodies, like rheumatoid factor and anti-cyclic citrullinated peptide antibodies. If you have pain in your foot or ankle joints, it is suggested that you schedule an appointment with a podiatrist for proper testing and a diagnosis so that the right treatment can be administered.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Handle a Long Work Day on Your Feet
In 2014, the American Podiatric Medical Association surveyed 1,000 American adults and found that half of all respondents lived with foot pain. Fortunately, there are ways to avoid foot problems such as following a daily footcare routine and wearing proper footwear at work.
If you have a job that requires you to be on your feet, it is best that you do not wear flat sole shoes. Your heel should be slightly elevated (less than 2 inches, but at least ¼-inch) if you are going to be standing for a prolonged period. You should also make sure that the shoes you wear are not too small. Tight shoes may cut off circulation to your feet, which will result in pain and blisters. It is always best to purchase fitted shoes later in the day, because the feet tend to swell as the day progresses. It may also be helpful to buy shoes a half size larger if you plan on wearing custom orthotics or arch supports.
Your muscles may become stiff when you are constantly standing up. It is important to take breaks every hour to stretch and relax. One tip is to perform calf raises, because this exercise will help improve your circulation. To perform this stretch, you first need to stand on the edge of a step with your abdominal muscles pulled inward. You then need to grip the step with the balls of your feet with your heels hanging over the edge. Next, try to raise your heels above the step by a few inches while standing on your tiptoes; hold this pose for a second. You should then lower your heels back even to the platform. These calf raises should be done ten times for full effectiveness.
You should also take care of your feet while you are at home. One of the best ways to prepare your feet for a long day of work is to soak them in ice water. Doing so for 20 minutes will help fight the swelling and inflammation that results from being on your feet at work.
Nevertheless, if you are experiencing pain in your feet, you should seek help from your podiatrist. Your doctor will help treat any ailments you may have in addition to helping you prevent any other ailments from developing in the future.
Protecting Your Feet in Chilly Work Environments

As the temperatures plummet and the outside environment becomes frosty, safeguarding your feet during outdoor work is paramount. Wearing proper footwear is the frontline defense against the biting cold. Choose insulated, waterproof boots that shield your feet from moisture and provide thermal protection. Layering socks is an effective strategy, ensuring warmth without compromising circulation. Choose moisture-wicking materials to prevent sweat accumulation, as dampness can intensify the cold. Additionally, ensure your boots are breathable to discourage moisture buildup. Regular breaks offer an opportunity to warm up and restore circulation. Invest in quality, insulated insoles to add an extra layer of warmth and comfort. Be mindful of frostbite warning signs, such as numbness or tingling, and promptly address any discomfort. Prioritize foot hygiene to prevent issues like frostbite and trench foot. If you are seeking additional tips on foot protection while working during the winter months, it is suggested that you confer with a podiatrist.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Warts Can Be Treated!
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Peripheral Artery Disease and Your Feet
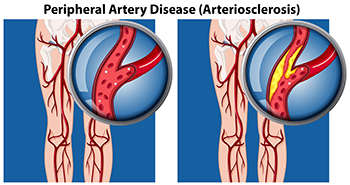
Peripheral artery disease, or PAD, is a condition that affects the arteries, causing narrowing and restricting blood flow, primarily to the lower limbs and feet. It is more prevalent among people aged 50 to 75, with more women than men affected. The hallmark symptom of PAD is intermittent pain in one or both calves during physical activity, which subsides with rest. This discomfort stems from the narrowed femoral artery, which hinders adequate delivery of blood and oxygen to calf muscles and feet during movement. Walking uphill or climbing stairs may intensify the pain. In severe cases, where blood supply is significantly reduced, individuals may experience pain, particularly at night. This type of pain typically is felt in the toes and feet. Other signs of peripheral artery disease include poor hair and toenail growth cool feet, and weak or absent pulses in the arteries of the feet. If left untreated, PAD can lead to complications such as skin ulcers and, in rare cases, gangrene. For that reason, if you believe you have developed peripheral artery disease, it is suggested that you schedule regular appointments with a podiatrist who is trained to manage symptoms effectively. A podiatrist can assess circulation, identify potential issues, and provide guidance on lifestyle modifications that can improve your overall foot health.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Health Implications of Cracked Heels

Cracked heels are not merely a cosmetic concern, their impact can extend beyond the surface, and may affect overall foot health and well-being. These painful fissures in the skin create an entry point for bacteria, increasing the risk of infections. As the cracks deepen, they can lead to bleeding and expose sensitive tissues, causing discomfort and hindering mobility. In severe cases, untreated cracked heels may contribute to balance issues, potentially increasing the risk of falls, particularly in older individuals. The pain associated with cracked heels can alter gait patterns, placing undue stress on other joints, such as the knees and hips. Moreover, the constant pressure on the feet can lead to chronic inflammation, exacerbating conditions such as plantar fasciitis. Addressing cracked heels involves more than cosmetic care, it is a vital aspect of maintaining overall foot health and preventing potential complications that can impact one's daily life and mobility. If you have cracked heels, it is suggested that you schedule an appointment with a podiatrist who can offer prescribed medication as an effective treatment method.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
Causes of Stress Fractures

Engaging regularly in high-impact activities, like basketball, running, or professional dancing, may expose you to the discomfort of a foot stress fracture. This overuse injury involves hairline cracks in weight-bearing bones of the foot. If left untreated, a stress fracture in the foot can escalate into a more serious concern. However, stress fractures are not always easy to diagnose. Pain upon weight-bearing activities that often subsides after rest is a primary indicator of stress fractures. Tenderness in the affected area, occasional bruising, and swelling around the ankle are other signs to be noted. Various factors contribute to the development of stress fractures in the foot. Overuse and repetitive stress, stemming from prolonged engagement in activities without adequate rest, can subject the foot bones to cumulative stress. Wearing inadequate footwear, whether ill-fitting or worn-out, further elevates the risk by providing insufficient support and shock absorption. Additionally, suddenly increasing the intensity or duration of physical activity can overwhelm the bones, especially without sufficient time to adapt. Nutritional deficiencies, particularly in calcium and vitamin D, can weaken bones and make them more susceptible to hairline fractures. If you believe you may have incurred a foot stress fracture, it is suggested that you make an appointment with a podiatrist for a thorough exam and suitable imaging tests and treatment options.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact Stephen Boykins, DPM from SoCal Podiatry, P.C.. Our doctor can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
- Gender – They are more commonly found in women compared to men.
- Foot Problems – People with unusual arches in their feet are more likely to develop stress fractures.
- Certain Sports – Dancers, gymnasts, tennis players, runners, and basketball players are more likely to develop stress fractures.
- Lack of Nutrients – A lack of vitamin D and calcium may weaken the bones and make you more prone to stress fractures
- Weak Bones – Osteoporosis can weaken the bones therefore resulting in stress fractures
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact our offices located in Downey and Moreno Valley, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.